A Pain In The BIG Toe!
Big Toe Pain
The great toe or 'Hallux' is the most important out of all the five toes!
It is pivotal to our forward propulsion during normal walking & running, & when painful, can impact our function and quality of life.
Though not receiving as much attention as some of the more high-profile joints like the hip and knee, Big toe osteoarthritis (OA) affects about 8% of the population aged over 50 years.
One of the hallmark signs of big toe arthritis is pain and an inability to push off during walking or running.
This can impact biomechanics- placing more stress on the structures on the outside of the foot.
This ailment is often ‘over imaged’ and can be more simply diagnosed with clinical tests. Patients will often present to the clinic with X-rays and ultrasound highlighting a change in their big toe joint but none the wiser to what they need to do fix this debilitating disorder.
This does not need to be the case!
The routine use of x-rays is not advocated in international OA guidelines, and contradicts recent recommendations which state that imaging is not required for a diagnosis in patients with a typical presentation of peripheral joint OA.
So what can we do to help?!?
There are many things that you can do to help this pain:
- Activity modification
- Decrease body mass
- Over the counter medication
- Mobilisation of the joint
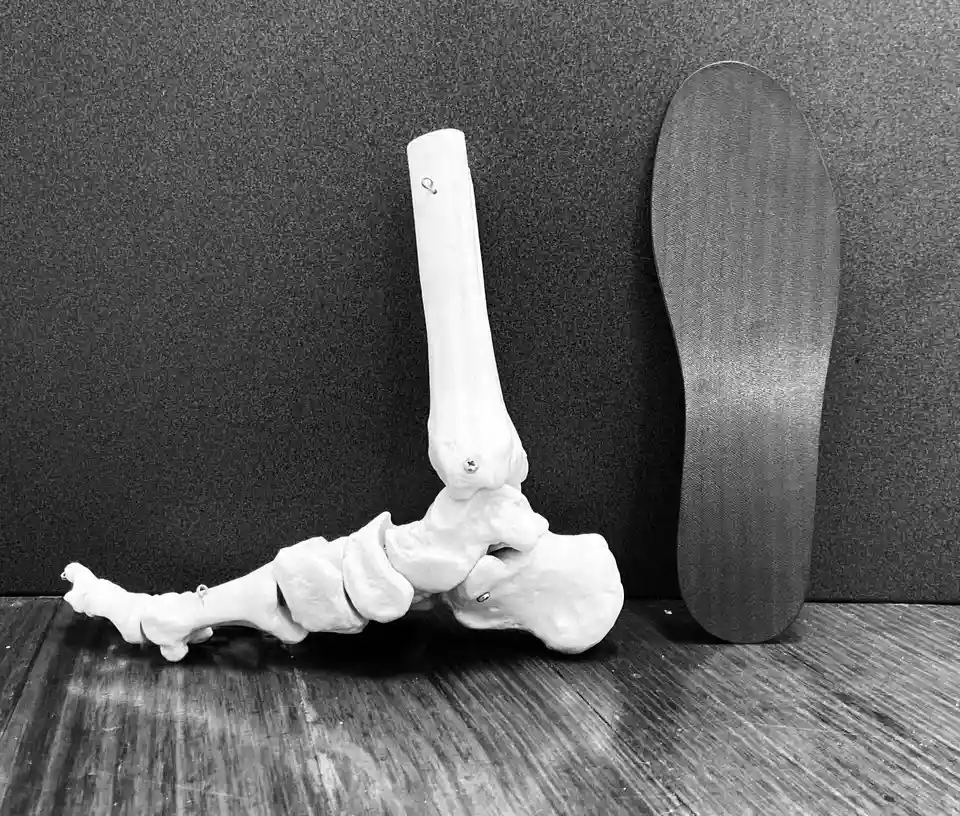
- Off the shelf foot orthotics
- Custom foot orthotics including carbon foot plates
- Footwear changes
- Footwear modification
- Exercise therapy
However two recent studies have found that the use of a rocker soled shoe in conjunction with a foot orthotic or the use of a carbon fibre foot plate have been effective in the treatment of Big toe pain.
So if you're battling to walk when first out of bed in the morning, get in touch with our podiatrist Sam to discuss your options.
Contact us on 03 9329 9988 or click https://bit.ly/3d4EB5U to schedule a time with Sam.