Plantar Fasciitis
A New Way to Deal with Heel Pain or Plantar Fasciitis
“That wretched heel pain just won’t go away!”
“I hobble out of bed in the morning and it feels like I’m walking on a pebble beach!”
Heel pain affects us across the lifespan but is more prominent across the fifth and sixth decades.
Sometimes a cause is easily identifiable – A sudden increase in running or walking activity, change in footwear or substantial gain in weight.
Sometimes things aren’t so clear.
The plantar fascia is like a thick ‘tendon like’ structure that runs under the arch of the foot. It attaches the toes to the heel bone and has continuity with the Achilles tendon.
There are many ways that clinicians can treat Plantar fasciitis or plantar heel pain.
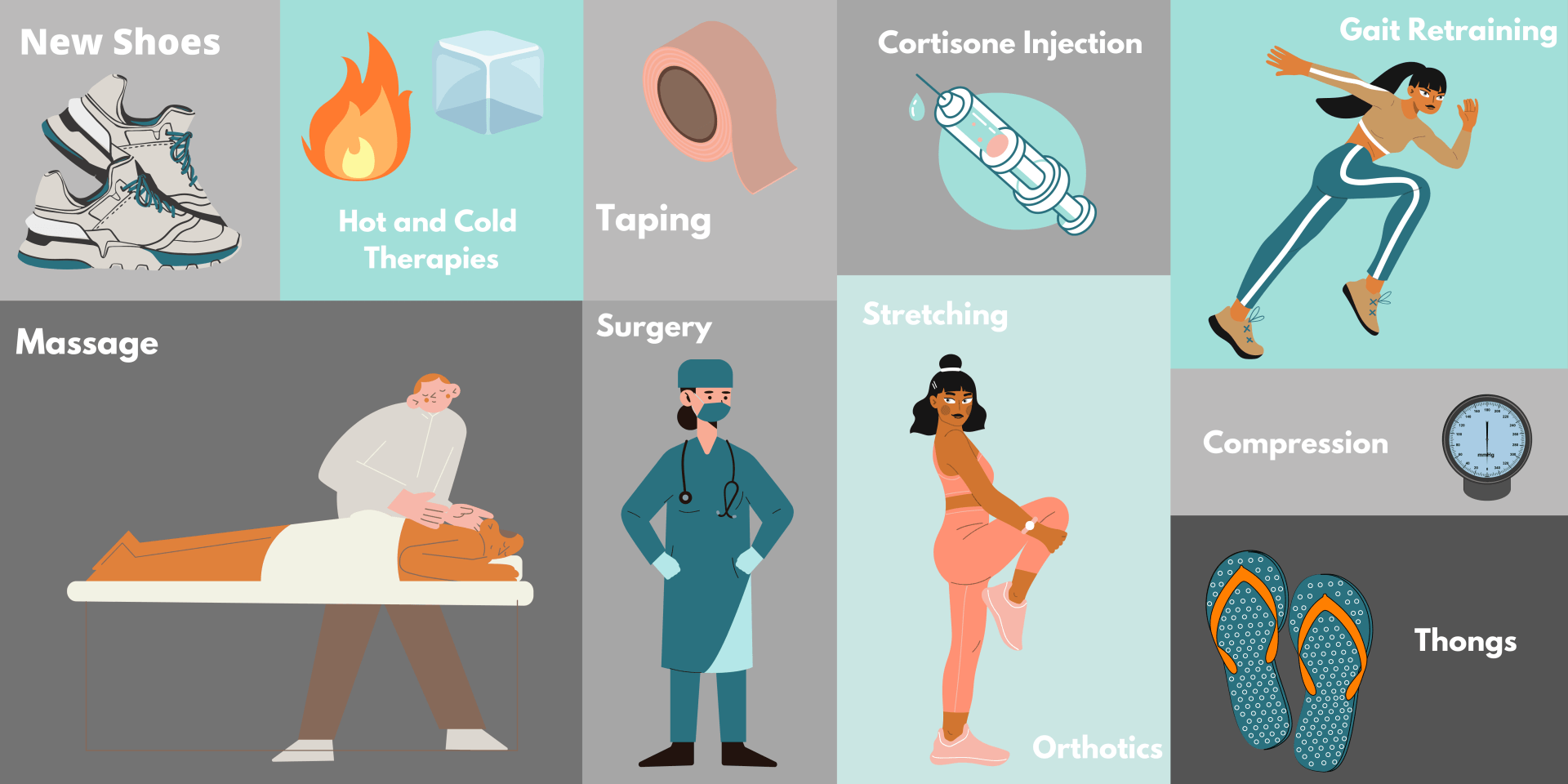
Some strategies might involve:
A quick google search will bring up 12,600,000 results and in a recent study there have been a reported 143 various treatments that are commonly used by clinicians. That seems to be a lot!!!
So how do we sift through the rubble to find the ‘treatment gold’?
Well…… several clever cookies lead by Michael Rathleff¹ (researcher from Denmark) used the principle of High Load Strength Training (HLST) for people with plantar fasciitis. This has been used for other conditions such as Achilles and patella tendinitis to great effect.
The researchers found…
“a simple progressive exercise protocol, performed every second day, resulted in superior self‐reported outcome after 3 months compared with plantar‐specific stretching. High‐load strength training may aid in a quicker reduction in pain and improvements in function.”¹
So it seems a strength program is the way to go…….
But not any old program just slapped together!
We need to ensure that the program is progressive – Adds extra load, hits the right number of sets, reps and frequency of sessions throughout the week
Errol Street podiatrist Sam & the remainder of the team have the experience required to get rid of your plantar fasciitis once and for all!
Call the clinic for more information.
References
- Rathleff, M. S., Mølgaard, C. M., Fredberg, U., Kaalund, S., Andersen, K. B., Jensen, T. T., ... & Olesen, J. L. (2015). High‐load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12‐month follow‐up. Scandinavian journal of medicine & science in sports, 25(3), e292-e300.