Why scans are not the answer!
Find out how MRI can be counter productive.
That niggling low back pain has persisted for months. You have tried various types of therapies & medications without a resolution!
You decide to get an expert opinion from your trusted GP.
“Doctor, should we get a scan to see what is going on?”
A common sequence of events that occurs with longstanding pain. Surely a scan will provide the answers, attribute a cause to the symptoms, and direct a pathway back to a healthy, active, pain free lifestyle.
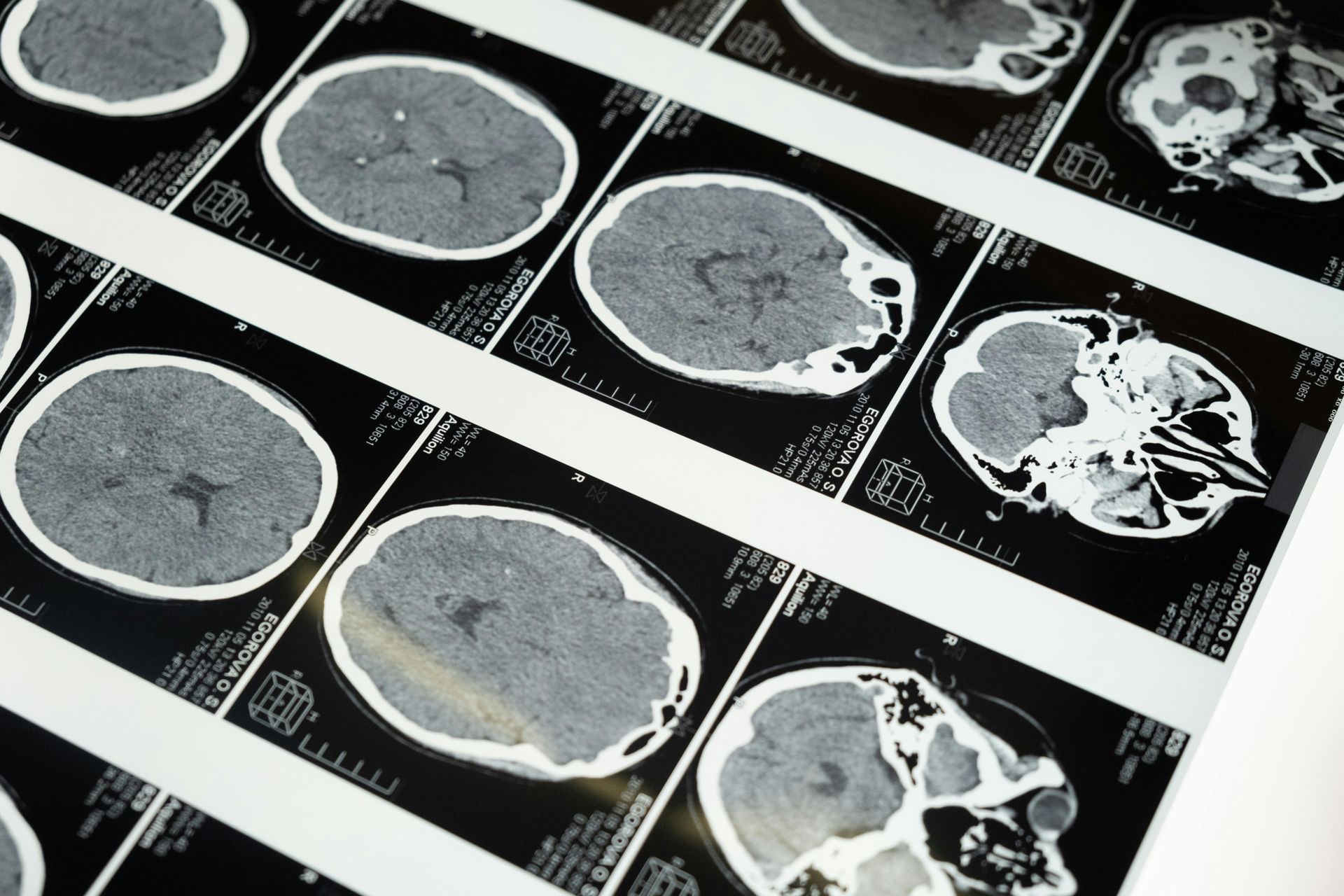
Over recent years, our understanding of the relationship between pain and abnormalities on an MRI, has evolved substantially. Traditionally, an episode of low back pain lasting for multiple weeks would end in an MRI – finding a disc bulge – and would direct a specific line of treatment to resorb or ‘unbulge’ the disc.
Recent studies have found that these abnormalities on MRI are not necessarily related to pain, but rather are related to the normal ageing process. One group of researchers found that in people without any pain, the likelihood of an MRI showing abnormalities increased the older we get.
90-95% of low back pain is what we consider non-specific - no specific structural cause- where 5-10% can present as a sinister pathology, and your clinician will be able to identify if you fit into this group.
A similar story exists with knee imaging. 115 pain free adult knees were scanned under MRI – 97% were found to have abnormalities of the bones, cartilage and ligaments! This further highlights the idea that what we see on imaging doesn’t necessarily explain the symptoms.
The negative consequences of imaging are two fold – the excesses of radiation that accompany Xray & CT scans can be harmful – combined with the fear and anxiety that is provoked when hearing of the damage inside our joints. The latter has been shown to contribute to worsening of symptoms and can prolong the pain experience.
While majority of injuries and pain states can be rehabilitated by identifying specific causes and intervening with the appropriate rehab strategies at the right time, it makes sense to avoid imaging!
Brinjikji W, Luetmer PH, Comstock, B et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am j Neuroradiol 2015: 36: 811-6
Horga, L. M., Hirschmann, A. C., Henckel, J., Fotiadou, A., Di Laura, A., Torlasco, C., D'Silva, A., Sharma, S., Moon, J. C., & Hart, A. J. (2020). Prevalence of abnormal findings in 230 knees of asymptomatic adults using 3.0 T MRI. Skeletal radiology, 49(7), 1099–1107. https://doi.org/10.1007/s00256-020-03394-z