Is it Safe to Exercise with Pain?
Now that we have learnt rest is not very helpful when addressing a long- term injury
Rest Is Not Best, you might have some questions -
- Should I continue to exercise if I have pain?
- Am I going to get worse if I continue to exercise with pain?
- Is pain a sign that something in my body is horribly wrong?
Very valid questions!
Read on and I’ll take you on a journey through the pain experience!
What is the role of pain?
The International Association for the Study of Pain (IASP) states:
"Pain is an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage"
So…..
Pain is unpleasant ……. Everyone who has burnt their finger on a stove top can attest to this!
Pain can be emotional…….. Kids (& some adults!) cry when they fall over and graze their knee.
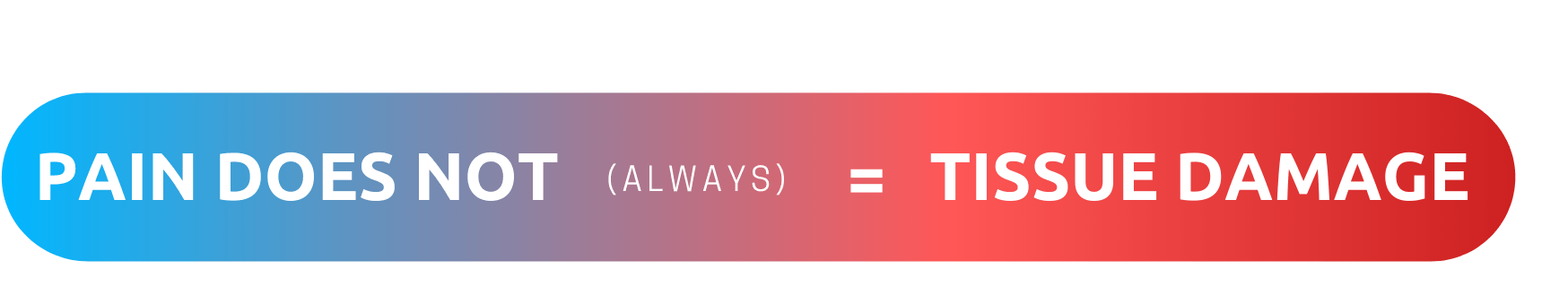
Pain is associated with ACTUAL or POTENTIAL tissue damage .
Potential tissue damage?
This insinuates that for pain to be present we don’t necessarily require damage to our body.
It could be a “perception’” of damage to the body.
This has been a major breakthrough in the pain research over the previous 20 years.
When we hurt ourselves acutely, for instance ….. A rolled ankle
- Ligaments stretch or tear – which sets off our danger sensors,
- Sending signals to the brain – Pain is developed.
- A protective mechanism to keep us safe – we limp or seek crutches to let the body heal.
Pain in this instance is our personal protector.
This is a great system to protect us from danger in the short term,
however what happens when we have pain that nags us for months or EVEN years?
Our once loyal bodyguard that protected us from danger betrays us!
The tissues have healed, but the brain still produces pain signals??
It is in this scenario that we use graduated exercise as our weapon against a malfunctioning pain system.
To learn more about the role that pain has in protecting us, watch this engaging talk by renowned pain researcher Lorimer Moseley.
https://www.youtube.com/watch?v=lCF1_Fs00nM
Now that we understand the basics of the pain system, we can use this to manage our pain during exercise.
Here are some signs that it is safe to continue to exercise in the presence of pain:
1. Your pain level is low - less than 4/10
2. You have had long term pain - Pain that has persisted for 6 months +
3. Your pain doesn’t get horribly worse during activity or the next morning
4. You have ruled out any potential structural or tissue based issues - Seek advice from your health professional.
Under these conditions, and over time, your brain will learn that its safe to exercise and your pain will slowly start to reduce.
This can take a long time!
So the next time you contemplating skipping a gym session because of a niggling long term knee injury, test yourself on the above criteria and show your brain who is boss!